You’ve heard the horror stories about healthcare data breaches — leaked medical records, hacked consultation platforms, stolen payment details, and massive legal penalties. When patient trust is your entire business, even a single security lapse can destroy everything overnight.
This is why the question “Is a white-label Lybrate app really safe?” is not just technical — it’s existential for healthcare entrepreneurs in 2025.
With millions of users now relying on telemedicine platforms for diagnosis, consultations, prescriptions, and payments, digital healthcare apps have become one of the most targeted sectors for cybercrime. Attackers no longer just chase financial data — they target sensitive medical histories, identity records, and insurance details that sell at a premium on dark web markets.
In 2025, governments have also tightened healthcare data regulations worldwide. Compliance failures now lead not only to fines but also criminal liability, platform shutdowns, and permanent reputational damage. This makes security no longer a “feature” — it is the foundation of your entire app business.
In this guide, we deliver a completely honest safety assessment of white-label Lybrate apps — no marketing fluff. You’ll learn:
- The real security risks in healthcare app platforms
- The exact compliance standards your app must meet
- How unsafe providers cut corners
- And how Miracuves designs security-first white-label Lybrate apps for long-term legal, technical, and business protection
This article will help you judge white-label healthcare app safety like a security professional — before you invest a single dollar.
Read more : – Best Lybrate Clone Script 2025 – Build a Profitable Telemedicine Platform
Understanding White-Label Lybrate App Security Landscape
What “white-label security” actually means
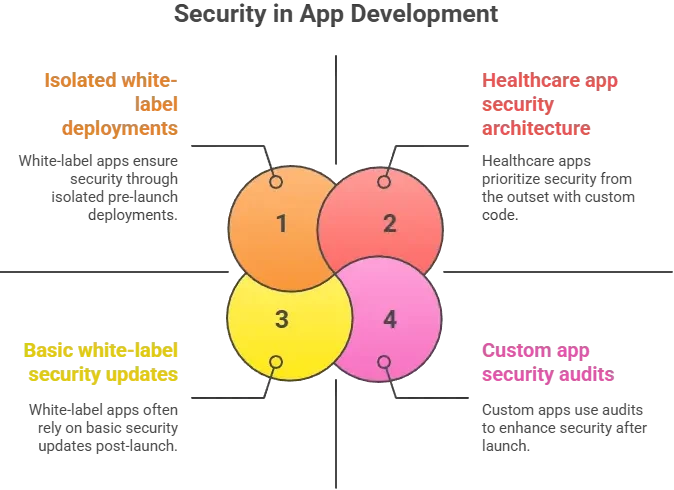
White-label security does not mean generic or weaker protection by default. It simply means the core app framework is pre-built and licensed for reuse, while security controls, hosting, compliance, and configuration are tailored for each business. The real safety of a white-label Lybrate app depends on how the provider engineers encryption, access control, infrastructure security, and regulatory compliance — not on the white-label model itself.
A secure white-label Lybrate app uses the same enterprise security layers as custom-built healthcare platforms, including encrypted databases, hardened cloud servers, secured APIs, and regulated data handling workflows.
Common security myths vs reality
Many founders assume that custom-built apps are automatically safer than white-label apps. This is one of the biggest misconceptions in healthcare technology.
Why people worry about white-label Lybrate apps
The concerns come from real global incidents where poorly built healthcare apps exposed:
- Patient consultation histories
- Diagnostic reports and prescriptions
- Payment and insurance information
- Identity documents and addresses
When entrepreneurs hear “white-label,” they fear shortcuts in encryption, shared databases, or weak compliance. These fears are valid only when the provider prioritizes speed and pricing over regulated security engineering.
Current threat landscape for Lybrate-type healthcare platforms
In 2025, healthcare platforms rank among the top three most attacked digital sectors globally, alongside financial services and government systems. Typical attack vectors now include:
- Ransomware targeting hospital and telemedicine databases
- API exploitation in doctor booking and payment flows
- Phishing attacks on doctors and admin dashboards
- Account takeover through weak authentication
- Data scraping through unsecured patient search endpoints
Healthcare data is now more valuable than credit card data on illegal markets because it enables long-term identity fraud and medical insurance abuse.
Security standards in 2025
Modern healthcare apps are now expected to meet security by design principles, including:
- Zero-trust network architecture
- Default encryption for data at rest and in transit
- Continuous vulnerability scanning
- Mandatory audit trails for all medical data access
- Role-based access controls for doctors, patients, and administrators
Security is no longer an optional upgrade. It is now an operational requirement embedded into healthcare platform architecture.
Real-world statistics on app security incidents
Recent global cybersecurity reports show:
- Over 45 percent of healthcare data breaches originate from application-level vulnerabilities
- Telemedicine platforms experienced a 69 percent year-over-year increase in cyberattacks
- More than 60 percent of breached healthcare apps were running outdated backend frameworks
- The average cost of a single healthcare data breach in 2025 exceeds USD 11 million including fines, lawsuits, downtime, and brand damage
These numbers explain why safety evaluation of a white-label Lybrate app must be as strict as that of a hospital information system.
Key Security Risks & How to Identify Them
Data Protection & Privacy Risks
User personal information
A white-label Lybrate app handles extremely sensitive personal data including patient names, contact details, age, medical conditions, consultation history, and prescriptions. If databases are not encrypted properly or access controls are weak, this data becomes vulnerable to leaks, insider abuse, and cyberattacks.
Payment data security
Healthcare platforms process consultation fees, subscription payments, and sometimes insurance-related transactions. If the app does not meet PCI DSS standards, payment tokenization is weak, or APIs are exposed, financial theft becomes a real risk for both users and platform owners.
Location tracking concerns
Doctor discovery, ambulance services, and appointment logistics often rely on live location tracking. If GPS data is stored without encryption or shared with unsecured third-party services, it can expose real-time physical movement of users and doctors.
GDPR and CCPA compliance
Improper consent management, lack of data deletion mechanisms, and unclear privacy policies can directly violate GDPR, CCPA, and regional health data protection laws. Non-compliance leads to heavy penalties, forced shutdowns, and legal actions against founders.
Technical Vulnerabilities
Code quality issues
Poorly written backend code, hardcoded credentials, and lack of secure coding practices lead to SQL injection, cross-site scripting, and authentication bypass vulnerabilities.
Server security gaps
Misconfigured cloud servers, open ports, weak firewall rules, and missing intrusion detection systems allow attackers to directly access backend infrastructure.
API vulnerabilities
Healthcare apps depend heavily on APIs for appointments, payments, video consultations, and notifications. Unsecured APIs enable data scraping, unauthorized access, and automated attacks.
Third-party integrations
Video hosting, SMS gateways, payment processors, analytics tools, and diagnostics systems all introduce risk if vendors are not security verified and integration keys are not properly secured.
Business Risks
Legal liability
A single data breach can trigger lawsuits from patients, doctors, and regulators. Founders become personally liable in many jurisdictions where negligence is proven.
Reputation damage
Trust is the currency of healthcare platforms. Once public confidence is lost, user churn increases rapidly and long-term brand damage becomes irreversible.
Financial losses
Beyond fines, businesses face downtime costs, ransom demands, legal defense costs, infrastructure recovery, and customer compensation.
Regulatory penalties
Health regulators can suspend operations, impose multimillion-dollar penalties, revoke licenses, and blacklist platforms from operating in certain regions.
Risk Assessment Checklist
Use this checklist to quickly evaluate white-label Lybrate app risk exposure:
- Is all patient data encrypted at rest and in transit
- Are role-based access controls enforced for doctors, staff, and administrators
- Are APIs protected with authentication, rate-limiting, and monitoring
- Is payment processing fully PCI DSS compliant
- Are user consent and data deletion workflows legally compliant
- Are third-party vendors security audited
- Is there an incident response and breach notification plan
- Are security logs retained and monitored continuously
- Are regular vulnerability scans and penetration tests conducted
If multiple answers are “no,” your platform carries high operational and legal threat exposure.
Read more : – Business Model of Lybrate : Complete Strategy Breakdown 2025
Security Standards Your White-Label Lybrate App Must Meet
Essential Certifications
ISO 27001 compliance
This international standard defines how healthcare platforms must manage information security, including policies, risk assessment, data handling, and access control. Any white-label Lybrate app provider must follow ISO 27001 frameworks for secure operations.
SOC 2 Type II
This certification evaluates continuous security controls, system integrity, data confidentiality, and uptime reliability. For healthcare apps handling sensitive patient records, SOC 2 Type II demonstrates long-term operational security discipline.
GDPR compliance
A mandatory requirement for apps serving users in or from the European Union. It governs consent, breach notifications, right-to-erasure, and secure data storage. A white-label Lybrate app must include built-in GDPR-friendly workflows.
HIPAA compliance
If the app serves the United States healthcare market or stores PHI (Protected Health Information), HIPAA rules must be implemented. This requires audit logs, secure transmission, role-based access, and strict data protection rules.
PCI DSS for payments
When handling card transactions for consultations or services, the app must comply with PCI DSS for secure payment storage, tokenization, and transmission.

Security Standards Comparison Table
| Requirement | Mandatory for Healthcare Apps | Recommended for All Apps | Purpose |
|---|---|---|---|
| ISO 27001 | Yes | Yes | Controls data protection and risk management |
| SOC 2 Type II | Yes | Yes | Ensures ongoing security and system integrity |
| GDPR | Yes (EU) | Yes | Protects user data and privacy rights |
| HIPAA | US only | Recommended | Regulates handling of medical information |
| PCI DSS | Yes for payments | Yes | Secures card transactions |
| End-to-End Encryption | Yes | Yes | Protects data from interception |
| Penetration Testing | Yes | Yes | Identifies vulnerabilities before attackers do |
| SSL Certificates | Yes | Yes | Secures data transmission |
Red Flags – How to Spot Unsafe White-Label Providers
No security documentation
If a provider cannot share formal security architecture documents, compliance reports, or audit summaries, it usually means security has never been properly implemented or verified.
Cheap pricing without explanation
Extremely low pricing often indicates shared databases, weak encryption, no penetration testing, and absence of compliance investment. In healthcare apps, low-cost setups are a major risk indicator.
No compliance certifications
Providers offering healthcare platforms without GDPR, HIPAA, ISO, or PCI references are exposing your business to immediate legal and operational threats.
Outdated technology stack
Old backend frameworks, unsupported server software, and legacy libraries create unpatched vulnerabilities that attackers actively exploit.
Poor code quality
Signs include slow systems, frequent crashes, weak authentication flows, and inconsistent behavior across modules. These are often symptoms of insecure coding practices.
No security updates policy
Security is not a one-time task. If a provider cannot explain how often patches, updates, and vulnerability fixes are deployed, your app will be vulnerable within months of launch.
Lack of data backup systems
Without automated encrypted backups and disaster recovery infrastructure, businesses face permanent data loss after cyber incidents, server failures, or ransomware attacks.
No insurance coverage
Serious providers carry cyber liability insurance and professional indemnity coverage. Absence of insurance means all risk is transferred directly to you.
Evaluation Checklist for Founders
Questions to ask providers
- How is patient data encrypted at rest and in transit
- What compliance standards does your platform currently meet
- How often do you conduct penetration testing
- How are API endpoints secured
- What is your breach response time commitment
- Do you provide audit logs for all medical data access
- Is data stored in isolated environments per client
Documents to request
- Security architecture diagram
- ISO or SOC audit reports
- GDPR data processing agreements
- Penetration testing summary reports
- Business continuity and disaster recovery plan
- Cyber insurance certificate
Testing procedures
- Perform independent vulnerability scans
- Test authentication and role-based access controls
- Validate data deletion and user consent workflows
- Run API abuse simulations
- Verify backup restoration processes
Due diligence steps
- Vendor background and breach history verification
- Legal review of data handling contracts
- Third-party security audits before launch
- Compliance mapping for target operating regions
- Infrastructure inspection of hosting environment
Read more : – Best Lybrate Clone Script 2025 – Build a Profitable Telemedicine Platform
Best Practices for Secure White-Label Lybrate App Implementation
Pre-Launch Security
Security audit process
Before your white-label Lybrate app goes live, a full security audit must be conducted across application code, APIs, servers, and database architecture. This identifies vulnerabilities early and prevents costly post-launch remediation.
Code review requirements
Every module handling patient data, payments, prescriptions, and communications must undergo secure code reviews. This ensures that insecure functions, weak validations, and unsafe data handling patterns are removed before production deployment.
Infrastructure hardening
Servers must be configured using hardened operating systems, firewalls, intrusion detection systems, segmented networks, private subnets, and restricted access controls. Public exposure of critical backend systems should be completely eliminated.
Compliance verification
All legal compliance requirements such as GDPR, HIPAA (if applicable), and PCI DSS must be validated before go-live. Consent flows, privacy policies, audit trails, and breach notification mechanisms must be tested and documented.
Staff training programs
Doctors, support teams, and administrators must be trained in secure access usage, phishing prevention, password hygiene, and data handling protocols. Human error remains one of the largest healthcare security vulnerabilities.
Post-Launch Monitoring
Continuous security monitoring
Security does not stop at launch. A secure white-label Lybrate app requires real-time monitoring of server activity, login attempts, API access patterns, and anomaly detection to identify threats before they escalate.
Regular updates and patches
Outdated frameworks and libraries are among the most common sources of breaches. Scheduled updates and emergency patch management must be part of the operational workflow.
Incident response planning
A defined security incident response plan must be in place, including detection, containment, forensic analysis, regulatory notification, user communication, and system restoration.
User data management
Data retention rules, consent expiry handling, secure deletion policies, and anonymization procedures must be monitored continuously to stay compliant with evolving privacy regulations.
Backup and recovery systems
Encrypted daily backups, geographically distributed storage, and tested recovery drills ensure that business operations can continue even after cyberattacks, ransomware incidents, or infrastructure failures.
Security Implementation Timeline
Week 1
- Security architecture design
- Infrastructure hardening
- Initial code security review
Week 2
- Compliance configuration
- Consent and privacy workflow implementation
- Payment security validation
Week 3
- Penetration testing
- API security validation
- Backup and disaster recovery setup
Week 4
- Final audit resolution
- Incident response simulation
- Production security sign-off
This phased approach ensures that a white-label Lybrate app launches with regulatory-grade security instead of reactive protection.
Legal & Compliance Considerations
Regulatory Requirements
Data protection laws by region
A white-label Lybrate app must comply with regional data protection regulations depending on where users and servers are located. These laws define how patient data is collected, stored, processed, and shared.
- India: Digital Personal Data Protection Act (DPDP Act) governs personal health information handling
- European Union: GDPR mandates strict consent, storage limitation, breach notification, and data subject rights
- United States: HIPAA governs the protection of electronic Protected Health Information (ePHI)
- Middle East and APAC: Local health data residency and cybersecurity compliance laws apply
Failure to comply with regional healthcare data laws can result in platform shutdowns, financial penalties, and criminal liability.
Industry-specific regulations
Healthcare apps must also follow medical council regulations, telemedicine guidelines, pharmacy compliance rules, and electronic health record standards applicable to their operating market.
User consent management
Legally valid consent must be collected for:
- Storing medical records
- Sharing data with doctors
- Processing payments
- Using location data
- Sending notifications and marketing communications
Every consent action must be logged and retrievable for audits.
Privacy policy requirements
Your privacy policy must clearly define:
- What data is collected
- Why it is collected
- How long it is stored
- Who it is shared with
- How users can request deletion
This document is legally enforceable and must be dynamically updated as regulations evolve.
Terms of service essentials
Terms must define user responsibilities, doctor liabilities, consultation limitations, dispute resolution mechanisms, refund policies, and jurisdiction of legal proceedings.
Liability Protection
Insurance requirements
Every healthcare platform must carry cyber liability insurance, professional indemnity insurance, and data breach coverage to protect against claims arising from system failures or security incidents.
Legal disclaimers
Telemedicine apps must include medical disclaimers clarifying that digital consultations do not replace emergency medical care and that diagnostic limitations may apply.
User agreements
Doctor and patient agreements must outline data responsibility, consultation obligations, payment terms, content use rights, and breach reporting commitments.
Incident reporting protocols
Healthcare laws require that breaches be reported within strict timelines, often within 72 hours. A structured compliance notification workflow must be implemented at both technical and legal levels.
Regulatory compliance monitoring
Compliance is not static. Laws change frequently. Continuous legal audits, policy updates, and staff training must be part of ongoing operations for any white-label Lybrate app.
Compliance Checklist by Region
India
- DPDP Act compliance
- Telemedicine Practice Guidelines
- Secure electronic health record storage
- Consent logging and audit trails
European Union
- GDPR lawful basis of processing
- Data subject rights management
- Cross-border data transfer safeguards
- Breach reporting within regulatory timelines
United States
- HIPAA Privacy Rule
- HIPAA Security Rule
- Business Associate Agreements
- Secure handling of ePHI
Middle East & APAC
- Health data compliance mandates
- Data localization rules
- National cybersecurity frameworks
Why Miracuves White-Label Lybrate App is Your Safest Choice
Miracuves Security Advantages
Enterprise-grade security architecture
Miracuves designs its white-label Lybrate app infrastructure using enterprise security principles including zero-trust access, isolated tenant environments, and hardened cloud deployments. Every client receives a dedicated, secured environment instead of shared risky setups.
Regular security audits and certifications
All Miracuves platforms undergo scheduled internal and third-party security audits. Vulnerability assessments, penetration testing, and compliance validation are part of the standard delivery process—not optional add-ons.
GDPR and regional compliance by default
Privacy-by-design architecture ensures built-in GDPR, DPDP Act, and region-specific compliance workflows including consent management, audit logging, data minimization, and right-to-erasure mechanisms.
24/7 security monitoring
Miracuves operates continuous monitoring across servers, networks, APIs, and authentication systems. Suspicious activity is detected in real time, reducing breach response time and minimizing exposure.
Encrypted data transmission and storage
All patient data, consultation records, prescriptions, and payment information are encrypted using industry-grade AES-256 and TLS 1.3 protocols both in transit and at rest.
Secure payment processing
PCI DSS-compliant payment gateways are integrated with tokenization, fraud monitoring, and transaction verification layers to ensure consultation payments remain fully protected.
Regular security updates
Security patches, framework upgrades, and dependency updates are released on a strict maintenance schedule to prevent exploitation of known vulnerabilities.
Cyber insurance coverage included
Miracuves platforms are backed by cyber liability and professional indemnity protection frameworks, adding an extra layer of financial risk mitigation for founders.
Security-First Value Proposition
Unlike many low-cost providers that prioritize speed over safety, Miracuves builds healthcare platforms with regulated security engineering at the core. This ensures long-term legal compliance, patient trust, platform stability, and scalable business protection.
With over 600 successful platform deployments across healthcare, fintech, marketplaces, and on-demand services, Miracuves maintains a zero major breach track record through proactive security governance rather than reactive fixes.
Conclusion
Do not compromise on security. Miracuves white-label Lybrate app solutions come with enterprise-grade security built-in. Our 600+ successful projects have maintained zero major security breaches. Get a free security assessment and see why businesses trust Miracuves for safe, compliant platforms.
In healthcare, security is not a technical checkbox — it is a legal, ethical, and business survival requirement. A white-label Lybrate app can be safe, scalable, and fully compliant only when built on regulated security architecture, continuous audits, and strict data protection practices. Choosing the right provider is not about features alone — it is about protecting lives, trust, and long-term revenue.
FAQs
1. How secure is a white-label Lybrate app compared to custom development?
Security depends on architecture and compliance, not on whether the app is white-label or custom. A professionally built white-label Lybrate app with ISO, GDPR, and HIPAA controls can be as secure as enterprise custom software.
2. What happens if there is a security breach?
Incident response protocols are activated immediately, affected systems are isolated, regulators are notified within legal timelines, and users are informed as required by law.
3. Who is responsible for security updates?
The platform provider manages core security updates, while the business owner must ensure operational policies and staff access controls are followed.
4. How is user data protected in a white-label Lybrate app?
User data is protected using end-to-end encryption, role-based access, secure databases, and audited access logs.
5. What compliance certifications should I look for?
ISO 27001, SOC 2 Type II, GDPR, HIPAA (if applicable), and PCI DSS for payments are essential.
6. Can a white-label Lybrate app meet enterprise security standards?
Yes, if it follows zero-trust architecture, encrypted infrastructure, continuous monitoring, and third-party audits.
7. How often should security audits be conducted?
At least once every quarter, with continuous vulnerability scanning running in real time.
8. What is included in the Miracuves security package?
Encrypted infrastructure, compliance-ready architecture, continuous monitoring, scheduled audits, secure payments, and disaster recovery systems.
9. How is security handled across different countries?
Compliance is mapped to each operating region with localized data protection and data residency controls.
10. What insurance is needed for app security?
Cyber liability insurance, professional indemnity insurance, and data breach coverage are mandatory for healthcare platforms.